This blog post was written by Jeni Nestler, LPC-IT, a Behavioral Health Therapist at the Beloit Area Community Health Center.
There are a lot of misconceptions around what depression is and is not
There are many depression-related myths and stereotypes floating around in society. These can be really discouraging for people that are struggling and can even prevent people from seeking help.
Described below are 5 common depression-related myths.
Depression only occurs after a sad/difficult event.
This is not true. Depression doesn’t always have a clear cause.
For example, imagine a teen that is struggling because they can’t see their friends during the COVID-19 pandemic. Imagine that this teen has a full belly, plenty of clothes, and their own room with a big, comfy bed. Both of their parents have been able to work at home with no trouble.
How might this teen feel if they were hungry? if their parent lost their job or housing? or if they were bullied at school? Do you think they would feel better or worse?
Our mental health depends not only on our biology, but our beliefs, life events, relationships, and societal forces.
Talking about depression or suicidal thoughts will make things worse.
The opposite is true! Talking about depression and suicidal thoughts can get us the help we need to feel better.
I could have prevented my depression if I only did _________.
Depression is not your fault. It’s not something you can prevent on your own.
Depression medications are addictive and harmful.
Anti-depressants are not addictive. Most of the time, people don’t notice any uncomfortable changes or side effects in their body.
However, there are some risks, and you should always discuss the potential risks with your doctor before taking any new medications, reducing your dose, or stopping your medication.
(Reference: Kim Nestler, MD/PhD; licensed psychiatrist (WI); Board certified in Psychiatry and Neurology)
Depression gets better on its own.
This is a really important one! Depression usually doesn’t get better on its own. Symptoms of depression are like flags that we need help. By knowing the different signs/symptoms of depression, were better able to get the help that we need.
So, what is depression? What are the signs, symptoms, and how does it affect us?
What is Depression?
Depression is an illness involving many chemicals in the brain. The chemicals involved in depression are different for each person, and what causes depression may differ for each person. Your depression is unique – specific to you.
Listed below are some common signs/symptoms of depression:
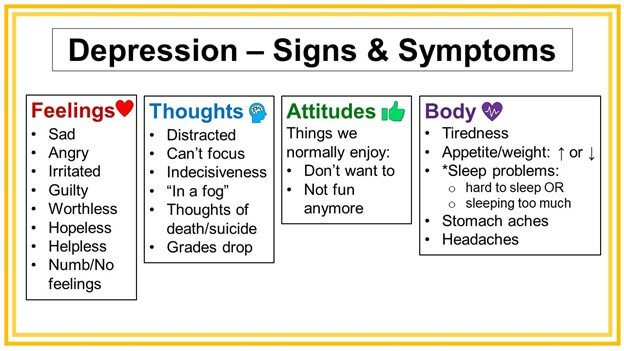
Depression can involve multiple combinations of the above symptoms (and others not listed), so your depression may look different from someone else’s depression. You might feel irritable and have trouble falling asleep, while another person feels sad, tired, and is sleeping too much.
How does depression affect our lives?
When we’re depressed, our daily tasks and responsibilities can seem really difficult. It might be hard to get up in the morning, get to work on time, or even brush our teeth.
Our feelings may be more intense or difficult to manage, and we might feel anxious – often times, depression and anxiety overlap. Approximately 50% of people with depression also have an anxiety disorder (Cameron, 2007).
Depression overlaps with trauma as well; about half of people with post-traumatic stress disorder (PTSD) also have major depression (Flory & Yehuda, 2015).
I think I may have depression – How can I get help?
Because the causes, chemicals, and symptoms of depression are different for each person, there’s no single cure or magic treatment that works for everyone – this is why it’s important to ask for help. At Community Health Systems, Inc. (CHS), we’ll do our best to connect you with services that match your unique needs.
If you’re experiencing symptoms of depression and would like to meet with a behavioral health provider, give us a call at 608-361-0311 to schedule your first appointment.
If you live outside the Rock County area, please schedule an appointment with your Primary Care Provider (your medical doctor) to discuss your depressive symptoms.
For Rock County residents and non-residents:
If you (or a loved one) have thoughts of suicide, self-harm, or harming another person – or if you have a plan to do so – please call 911.
References
- American Foundation for Suicide Prevention. (2018, October 26). WHAT DO YOU KNOW ABOUT DEPRESSION IN TEENS? PRE-QUIZ [Pre-Quiz for Teen Suicide Prevention].
- Cameron, O. G. (2007). Understanding Comorbid Depression and Anxiety. Psychiatric Times, 24(14).
- Diagnostic and statistical manual of mental disorders: DSM-5. (2017). Arlington, VA: American Psychiatric Association.
- Flory, J., & Yehuda, R. (2015). Comorbidity between post-traumatic stress disorder and major depressive disorder: Alternative explanations and treatment considerations. Treatment of Affective Dysfunction in Challenging Contexts, 17(2), 141-150. doi:10.31887/dcns.2015.17.2/jflory
- Group Interpersonal Therapy (IPT) for depression. (2016). Geneva: World Health Organization.
- More than sad: Facts about depression in teens. (2018). Retrieved March 5, 2021, from https://www.bcbe.org/cms/lib/AL01901374/Centricity/Domain/467/factsaboutdepression.pdf
- Valente, D. (n.d.). More Than Sad: Suicide Prevention Group for Teen Depression [Psychotherapy curriculum based on American Foundation for Suicide Prevention More Than Sad resources]. Woodside, New York.